D4P: Exploring the Immune Response in Patients with COVID-19
D4P webinar streamed April 15, 2020
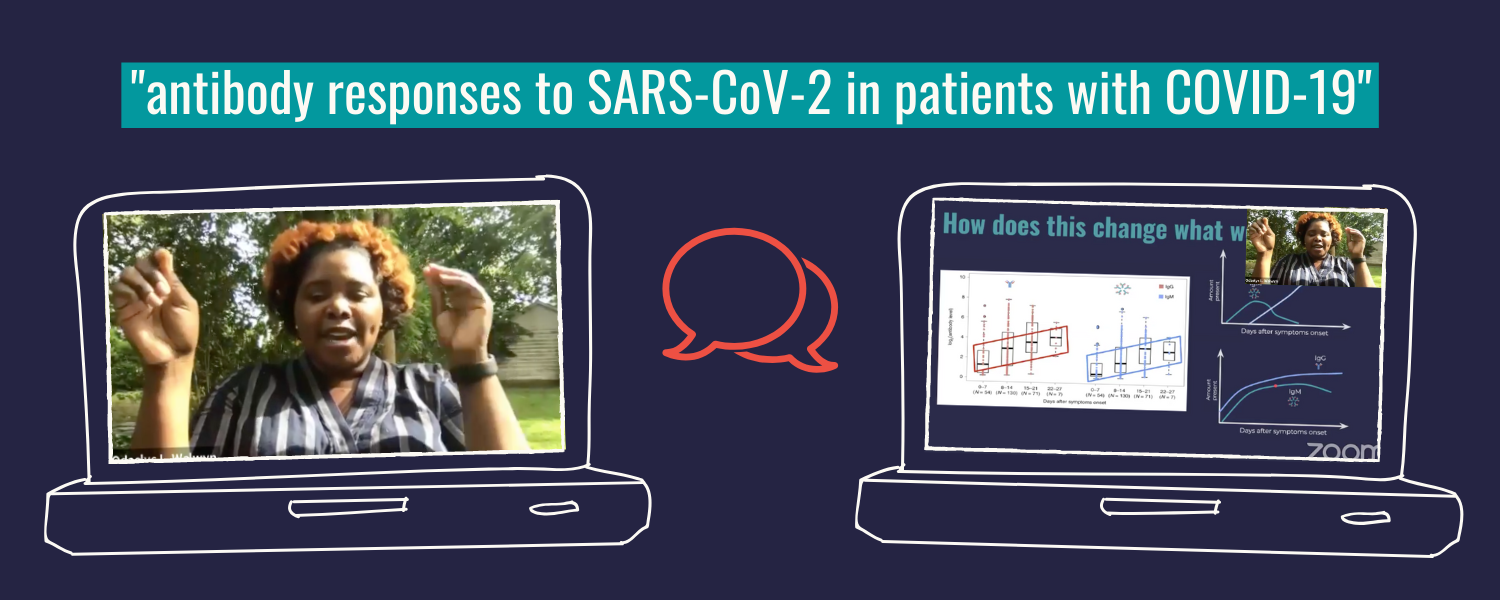
Paper: Antibody responses to SARS-CoV-2 in patients with COVID-19
The accompanying discussion guide is coming soon!
The recency of COVID-19 has made it difficult to fully grasp how human immune systems respond to the SARS-CoV-2 infection. Yet, in order to create an accurate picture of COVID-19’s impact on society and design appropriate serological tests, this information is critical. It is clear that humans are producing antibodies against this virus. However, we still need to understand the specific types of antibodies being made, and how long after infection can we expect our bodies to make them. Our D4P Fellow, Dr. Odaelys Pollard, presents data from the paper, “Antibody responses to SARS-CoV-2 in patients with COVID-19,” which chronicles the antibody response from 285 COVID-19 patients, and suggests a set of criteria for confirmation of infection.
The style of scientific reasoning used in this paper:
What you need to know:
Information is power, and when it comes to the COVID-19 pandemic, that information must come in the form of testing! The current approach to learning about an existing infection involves looking for the presence of SARS-CoV-2 RNA via a technique called RT-PCR (described in this previous D4P talk). While this approach is effective, there are instances of false negatives (people who test negative, but are actually infected with SARS-CoV-2). The authors of this paper suggest that antibody testing could complement the RT-PCR testing to help reduce the number of false negatives, and ultimately assist in controlling spread. However, we know very little around when, or at what level, antibodies specific to SARS-CoV-2 are being produced after initial infection. While this study reports on a small patient sample from a single geographical region, it is providing clues into the human immune response to SARS-CoV-2.
The following are the key terms defined in this D4P presentation, and are important for understanding the data presented by Dr. Pollard.
Antibodies
Antibodies are proteins produced by our immune cells (b lymphocytes) in response to infection. These molecules engage in a chemical interaction with a specific component found on a “foreign” invader, such as a virus, in order to get rid of it.
Human produce 5 classes of antibodies (IgM, IgG, IgA, IgD, and IgE). The researchers from this study report that IgM and IgG are the major classes of antibodies that are produced in response to the SARS-CoV-2 infection. More specifically, the researchers explore when IgM and IgG are detected in patients over the clinical course of COVID-19 (up to 4 weeks), as well as the amount of each antibody class that is produced.
Antigens
An antigen is a specific molecular piece of a “foreign” invader, such as a virus, that turns on our immune response, and is recognized by an antibody.
To leverage the natural biology inherent to the SARS-CoV-2 infection, researchers try to mimic the antigenic qualities of the virus when creating serological (antibody) tests. For example, both the “S” and “N” proteins from SARS-CoV-2 have been shown to bind to human antibodies. In this paper, the researchers used a fusion construct that combined the “S” and “N” proteins to capture antibodies in patients with COVID-19. They did this with a “fancy” version of an ELISA, called “Magnetic Chemiluminescence Enzyme Immunoassay” (MCLIA). You can learn more about ELISA technology in Dr. Pollard’s first D4P presentation.
Seroconversion
When we consider using blood to test for the presence of antibodies against SARS-CoV-2, we are really using serum as the input. Serum is the liquid component of the blood that does not deal with clotting, but includes components like antibodies, hormones, electrolytes, etc. Seroconversion refers to the point at which specific antibodies, such as those produced in response to SARS-CoV-2, go from being undetectable in serum, to being detectable in serum.
In this paper, the researchers were able to explore exactly when seroconversion took place in a subset of their patients who tested positive via RT-PCR, but did not yet mount an immune response.
Aggregate vs. Individual Data Points
Aggregate data is the compilation of many data points to produce a trend or identify a pattern for comparison. This is in contrast to individual data points, which allow for personalization. In this paper, the researchers used aggregate data to identify a general timeframe for seroconversion, and individual data points to explore the feasibility of combining the RT-PCR test with antibody testing to produce a more accurate diagnosis.
Research Updates
This presentation also referred to a recently published pre-print that explored the human antibody response in greater detail. You can find this article here.
About Our D4P Fellow
Odaelys Walwyn Pollard, PhD (she/her)
Dr. Pollard is the scientist educator for RockEDU Science Outreach. Before joining RockEDU, Odaelys worked on a variety of different initiatives around science education and outreach, and is a champion for equitable access to science. Odaelys is a trained microbiologist/immunologist, having earned her PhD at New York Medical College, in Westchester NY.